
EMPOWERING
PATIENTS
How Price Transparency Will
Lower Healthcare Costs
BY MIRANDA SPINDT & WILL FLANDERS, PHD
OCTOBER

Executive
Summary
WILL FLANDERS, PHD
RESEARCH DIRECTOR
Flanders@will-law.org
MIRANDA SPINDT
POLICY ASSOCIATE
Miranda@will-law.org
Empowering Patients
1
The Wisconsin Institute for Law & Liberty (“WILL”) exists to
advance the public interest in the rule of law, individual liberty,
constitutional government, and a robust civil society.
Healthcare costs have skyrocketed around the
country in recent years. Wisconsin is no exception
to this trend, with recent research finding that
the state has the fourth highest hospital costs
in the country. Coupled with inflation across the
economy at large, many Wisconsin families worry
about being able to pay their medical bills. Under
the Trump administration, there was an attempt
to introduce more market forces to the healthcare
industry by requiring that the prices for common
procedures be posted publicly, but compliance
remains low with this measure.
Healthcare is one of the only sectors of our
economy where consumers are expected to
purchase a good or service without knowing the
ultimate price. Price transparency works under
the theory that pricing information is a vital
component of the free market. Just as we can
compare the costs of gasoline at various stations
or cars at various dealerships, consumers ought
to be able to compare the cost of common
medical procedures at providers in their area. In
this report, we explore the possibility of bringing
healthcare price transparency to Wisconsin.
Among the key takeaways:
• Prices on shoppable services vary
extensively. For example, A CT scan
ranges from about $858 to $2,803 within
Wisconsin. This price variation means that
better information on prices could lead to
real savings for patients and businesses that
provide insurance to employees.
• 28% of workers are on High Deductible
Health Plans (HDHP) that incentivize
shopping around. High Deductible Plans,
often coupled with Health Savings Accounts,
require patients to cover a larger share of
the actual cost of their care. This means that
consumers have more potential to gain from
seeking out lower costoptions.
• Research suggests transparency can
work. Studies of insurance companies and
states that have implemented transparency
measures have found significant savings
forconsumers.
Policy makers should consider:
• Implementing full price transparency.
Require that healthcare providers and
insurance companies work together to
create a website where consumers can see
the “out-the-door” price at every provider
in the state for a list of common shoppable
procedures under their insurance.
• Creating incentives for shopping. Some
states have implemented systems that
require insurers to share savings with
consumers when a lower cost option is
chosen. This gives consumers additional
incentive to weigh the cost versus quality of
every potential provider.
Photo by Matheus Ferrero

Introduction
With healthcare costs consuming almost 20%
of our national GDP,
1
these spiraling costs have
become a considerable concern for individuals
and families all over the country. One in five
American households are in healthcare debt,
2
and about half of those report that it came from
unexpected medical bills.
3
A Kaiser Family
Foundation poll found that 67% of people worry
about unexpected medical bills which is more
than the percentage who worry about basic
necessities such as rent, food and gas.
4
Even
25% of Americans have reported delaying
treatment for a serious medical condition
because of cost.
5
This is likely even more true
in Wisconsin, which recent research has found
has the fourth highest hospital prices in the
nation.
6
With the crippling costs of healthcare
leading hardworking people into debt or to avoid
getting treatment in the first place, it is clear that
solutions are desperately needed across the
country and in Wisconsin.
Perhaps the most eicient way to address
these rising healthcare costs is to introduce
free-market mechanisms into the healthcare
sector. Competition and consumer choice are
the best ways to incentivize high-quality care
at lower prices. If consumers are given clear
pricing information about their medical goods
and services before ever getting treatment, they
would be empowered to make better decisions
about where they receive their healthcare.
When consumers are equipped to respond to
healthcare prices, there will be a meaningful
eect in reducing the cost of healthcare.
Photo by Nataliya Vaitkevich
2
Empowering Patients
Wisconsin has the 4th highest
hospital prices in the nation.

Empowering Patients
3
The Problem
When a patient seeks medical treatment, they are
often unaware of what their cost of care will be at the
end of the day. Hospitals, insurance companies, and
other third-party negotiators create deals, mostly in
secret, to determine the cost of a service and how
much of that cost will be paid for by the consumer.
As a result, the same procedure can have vastly
dierent costs from hospital to hospital and even
from patient to patient. For example, a CT scan of the
head can range in price from about $858 to $2,803 in
the state of Wisconsin.
7
This dierence in cost might
make sense if the treatment were better quality, but
there is often no correlation between higher costs
and higher quality of care or outcomes.
8
Instead,
what consumers pay is determined by what the
insurance company and hospital agreedupon.
Costs can get especially out of control when a
patient receives a surprise bill for out-of-network
care. While this usually happens in emergency
situations, it is possible for shoppable procedures
as well when a patient gets care from a facility or
provider that does not have an agreement with
their insurance company. If the insurance company
and the out-of-network hospital or provider cannot
reach an agreement on cost, they will pass on the
entirety of the bill to the patient. It is important to
note that this doesn’t just happen when a consumer
chooses to go to out-of-network facilities. Instead,
sometimes out-of-network services are provided at
in-network facilities,
9
making it nearly impossible for
consumers to make decisions about what healthcare
provider will result in the lowest cost. About 57% of
Americans have received a surprise medical bill, and
it is the most common reason for medical debt.
10
Photo by Drew Hays
A CT scan can range from
$858 to $2,803 in Wisconsin.

4
Empowering Patients
Photo by National Cancer Institute
Price Transparency
and the Free Market
4
Empowering Patients

Empowering Patients
5
To address the issue of rising costs and surprise
billing, many states across the nation have passed
price transparency laws, which make information
on pricing more readily available to consumers.
This enables the consumer to know what they will
pay for their healthcare before they receive it, not
after, giving consumers the opportunity to shop
for their scheduled treatments and procedures.
Not only will this help consumers save money, but
hospitals, providers, and insurance companies
will be incentivized to compete to provide the best
quality care at the lowest price possible. Consistent
with the free-market principles we see as being
eective in most other areas of the economy, this
competition should work to drive down overall
healthcare costs.
Typically, healthcare is considered an inelastic
good, meaning that a consumer will seek out
medical care regardless of the cost. This is in
contrast to most other consumer markets where
we may decide to buy less or seek alternatives due
to price increases. While High Deductible Health
Plans (HDHP) have become more common, for
many, third-party payers like insurance still cover
a large portion of our healthcare costs, meaning
there is a reduced incentive to know what we
will be paying for services before receiving them.
When hospitals and insurance companies are able
to keep patients in the dark, incentives change.
They can negotiate prices that are higher than
the cash price of the service, and the price for the
same service can vary widely depending on the
hospital, the provider, and the insurance company
a patient uses.
11
* For 2022, the IRS defines a high deductible health plan as any plan with a deductible of at least $1,400 for an individual or
$2,800 for a family. An HDHP’s total yearly out-of-pocket expenses (including deductibles, copayments, and coinsurance) can’t
be more than $7,050 for an individual or $14,100 for a family. (This limit doesn’t apply to out-of-network services.)
Source: https://www.healthcare.gov/glossary/high-deductible-health-plan/
In situations such as sudden illness or accident, a
patient will seek out medical care no matter what
it costs. Insurance is meant to financially protect
us from the cost of this type of catastrophic
care. However, about 80% of healthcare goods
and services are “shoppable” meaning that the
decision of where to get treatment does not
have to be made immediately.
12
This includes
services such as CT scans, blood tests, and
psychotherapy. It is these non-emergency
procedures where out-of-pocket price information
can be available for the consumer to decide
where to be treated for the best price.
As alluded to earlier, changing trends in
employer-sponsored health-insurance plans
also provide a strong incentive for greater
transparency. In an eort to control healthcare
costs, many employers have begun transitioning
their employees to HDHP paired with a
supplemental Health Savings Account (HSA).*
Since their inception in 2004, high deductible
plans have grown in popularity, covering about
28% of workers in 2021.
13
A 2020 study
14
found
that the average deductible for an individual was
now more than $4,000 and more than $8,000
for a family. Under these plans, individuals often
bear a greater share of health-care costs, and
consequently ought to be more incentivized to
shop for services.
80% of healthcare goods
andservices are shoppable.

6
Empowering Patients
Are Transparency
Measures Eective?
Photo by Anna Shvets
6
Empowering Patients

Empowering Patients
7
While the benefits of price transparency seem
clear in free-market theory, it is important to
consider whether they work in practice before
creating new requirements for the healthcare
industry. Of course, it is diicult to know whether
measures will be eective before they have been
tried. Outside of a few examples that will be noted
below, private sector compliance remains low with
federal requirements put in place under the Trump
administration requiring price transparency.
15
Despite a lack of nationwide implementation,
a small body of research has examined more
localized eorts at pricetransparency.
Some research has been conducted by
examining price transparency within the private
sector. One such study of the employees of a
national restaurant chain found that employees
who sought pricing information were able to
lower their costs by about 1.6%.
16
However,
these price-lowering eects were mitigated by
insurance. Of course, such tools are only eective
to the extent that consumers utilize them. One
study of AETNA’s private online pricing tool found
that only about 3.5% of consumers utilized the
tool, but those consumers that did saved more
Photo by Gratuit
than 12% on average for the same procedure.
17
The low utilization rate may be due to lack of
awareness
18
and diiculty using the available
tools,
19
which we believe can be remedied
through legislative and market-driven action.
Moving to studies of state-implemented
transparency programs, a 2019 policy report
from the Wisconsin Institute for Law and Liberty
(WILL)
20
brought together data on the cost
to consumers of healthcare in each state with
data on whether the state had a solid price
transparency law. The results suggested that
having poor transparency laws was correlated
with more residents reporting that they went
without care in the past year because of the cost.
A peer-reviewed study
21
of New Hampshire’s price
transparency system reached similar conclusions.
Looking at the time frame immediately before
and after the creation of a price-transparency
website, the author found that transparency led to
a significant shift toward lower-cost providers, and
a lowering of overall costs for both consumers and
insurers. The study estimated that savings were
about $7.9 million for patients and $36 million for
insurers over the time period of study.

8
Empowering Patients
Price Transparency
Around the Nation
Photo by Andrea Piacquadio
8
Empowering Patients

Empowering Patients
9
Price transparency rules have been enacted
at the federal level, but there has not been
significant compliance with the rules to yield
desired results. In 2019, President Trump signed
an executive order directing his administration
to implement price transparency regulations
which went into eect on January 1, 2021.
22
This
specific rule requires hospitals to post list prices
and negotiated prices for nearly all goods and
services oered. This information must be oered
in a machine-readable format and a consumer-
friendly display.
There is little guidance on what qualifies as
a “consumer friendly” format. As long as it is
searchable and on a publicly available website,
hospitals have the flexibility to decide what
format they use.
23
Unfortunately, this means that
understanding how to use the tools available can
still be diicult and hard to understand. Some
private sector and non-profit organizations have
taken on the task of collecting hospital price
data and making it more intuitive, in an attempt
to overcome these shortcomings. For example,
Turquoise Health
24
allows consumers to search
hospital prices by procedure and zip code, and
Sage Transparency
25
shows a comparison of
hospital prices relative to Medicare costs.
Another issue is that the “list prices” that
hospitals post may bear little relationship to
the final out-of-pocket cost the consumer pays.
To know what a consumer will pay, consumers
also need to know how much their insurance
company will cover for each service. To help
address this side of the transparency equation,
a second rule went into eect on July 1, 2022
26
to hold most group health plans of issuers of
group or individual health insurance to the similar
price transparency requirements. In a machine-
readable file, they must disclose the rates for
all covered items and services between the
plan or issuer and in-network providers. They
must also disclose the amounts allowed for, and
billed charges from, out-of-network providers.
Requirements for an online tool to disclose the
prices of 500 items and services will go into
eect in 2023, and that will change to include all
items and services in 2024.
These are steps in the right direction, but it is
diicult for the federal government to police
compliance across the nation. For the federal
hospital rule, the penalty increased in January of
2022 from $300 a day to a maximum of $5,500
a day.
27
However, an August 2022 study found
that only 16% of sampled hospitals were fully
complying with the regulation, including only
21% of Wisconsin hospitals.
28
It remains to be
seen how insurance company rule compliance
will fare. Indeed, the Foundation for Government
Accountability recently filed a lawsuit against
the Centers for Medicare and Medicaid Services
for failing to enforce compliance with the
federalrules.
29
Additionally, Congress passed the “No Surprises
Act” which went into eect on January 1, 2022.
30
This law protects patients from surprise billing
by requiring insurance companies to cover out-
of-network claims the same way they would for
in-network claims, and they cannot charge more
than in-network claims. It also establishes a
dispute resolution plan in the case that provider
and insurance company are not able to come to
an agreement on their own. This ensures that the
best interest of the patient comes first.

10
Empowering Patients
What Other States
Have Done
Photo by Olga Guryanova
10
Empowering Patients
Empowering Patients
11
FULL PRICE
TRANSPARENCY
States with complete price transparency require
cost estimates from all providers and insurance
carriers in virtually all instances, most closely
resembling the federal rules on price transparency.
However, how that information is delivered
varies from state to state. For example, providers
and insurers must provide price information
within two business days upon patient request
in Massachusetts,
31
whereas Alaska
32
and
Minnesota
33
require it within 10 business days.
In Texas, they take it a step further than other
states by also requiring user-friendly websites and
having stronger enforcement mechanisms.
34
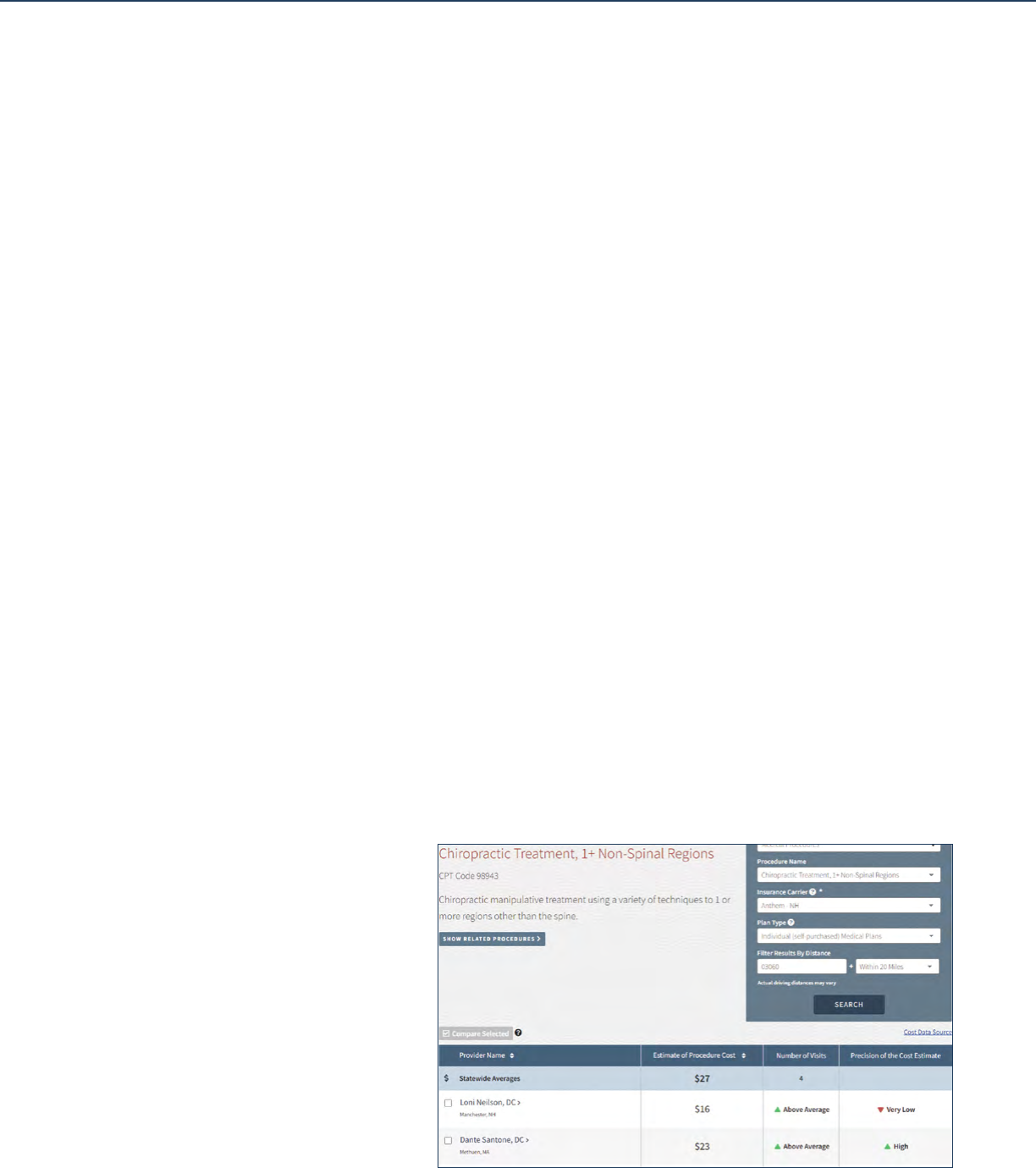
An example of how a price transparency website
could look is included in Figure 1 from New
Hampshire. New Hampshire was a pioneer in
providing pricing information to consumers,
with a website that predates the federal law on
the subject. The New Hampshire Department of
Insurance runs their state website which uses
insurance information to estimate the cost of over
120 procedures. The site allows a consumer to
pick between medical or dental care, input their
insurance company, and choose a procedure to
receive an estimate for the out-of-pocket cost
ofcare.
In Figure 1, we have searched for chiropractic care
with Anthem insurance within 20 miles of a ZIP
code in Nashua. The website returns the statewide
average cost of the procedure, as well as the typical
number of visits required for treatment. This is
followed by the cost at various providers within the
Nashua area. Note that these are cost estimates
based on data that has been collected in the state’s
All Payer Claims Database (APCD). The precision
of the estimate is based on the amount of data
points they have for that provider. In this case, the
estimate is more precise for Dr. Santone than it is
for Dr. Neilson. The information they can provide
is more personalized than a general estimator
tool, but it is not guaranteed that they have all the
necessary information to give an accurate out-
of-pocket cost to the consumer. In Washington, a
similar website was established by the state’s Oice
of Financial Management and oers cost estimates
for about 85 procedures based on ZIP code.
Figure 1.
New Hampshire Price
Transparency Example

12
Empowering Patients
While this may be a more desirable standard
for state law, even states with complete price
transparency do not necessarily have an easy
and accessible way for consumers to receive the
price information for the laws to be eective.
PARTIAL PRICE
TRANSPARENCY
States with partial price transparency require
price transparency for providers, hospitals
or insurance, but not all of them. Florida,
for example, requires hospitals to give cost
estimates within seven days upon request, but
not providers or insurance companies.
35
On the
other hand, Tennessee requires out-of-pocket
cost estimates be provided by insurance carriers
through a public website,
36
and Nebraska
requires cost estimates from providers for
uninsured and self-pay patients.
37
LIMITED PRICE
TRANSPARENCY
Limited Price Transparency describes states
which have price transparency requirements for
either providers or insurers, but only in certain
situations. For example, cost estimates in New
Jersey are only available if a non-emergency
procedure is scheduled in advance or if it is
out-of-network, and must be provided before
the appointment.
38
In Montana, patients are
* https://www.hcinnovationgroup.com/population-health-management/article/21118480/liberating-data-in-wisconsin-how-the-
state-is-evolving-its-allpayer-claims-database
only entitled to price information within ten
days of the request if the treatment is greater
than $500.
39
California exclusively requires cost
estimates for those who are uninsured, but
does not enforce responsiveness.
40
Additionally,
California requires hospitals to post the average
charges of the 25 most common inpatient and
outpatient procedures to their website, and
update ityearly.
41
NO PRICE
TRANSPARENCY
Unfortunately, a majority of states still have no
price transparency laws on the books. Some of
them do have some kind of price transparency
tool, however, it is not considered to be helpful
enough to help empower the consumer.
Wisconsin is among the states that currently do
not have laws mandating price transparency,
however a pair of private organizations operate
voluntary tools. The Wisconsin Hospital
Association operates a tool called Price Point,
42
which gives the median price charged for
procedures at individual hospitals, but does not
have the information needed to give accurate
out-of-pocket estimates. The Wisconsin Health
Information Organization operates the state’s
independent All-Payers Claim Database,
which collects claims data from insurers,
self-funded employers and the state to cover
approximately 75% of Wisconsin’s population.
*
These capabilities could serve as a baseline
for an eventual implementation of a universal

Empowering Patients
13
transparency measure. There are still about
17 states that do not have any laws or price-
transparency tools.
ANOTHER OPTION:
LOW-COST-SEEKING
INCENTIVES
Some states oer a shared savings program that
incentivizes consumers to choose lower-cost
healthcare services in non-emergency situations.
When a patient chooses lower-cost services, it
may result in savings for the insurer or provider,
which is then shared with the patient through
rewards such as a reduction in copayments,
credits toward a deductible, or cash. In Florida,
there is a shared savings program that is
available to full or part-time state employees on
the State Group health plan.
43
The program is
run by the Department of Management Services,
and the benefits are automatic when enrolled
in the State Group health plan. Enrollees can
use the Healthcare Bluebook
44
to search for
rewardable services or a bundled service from
SurgeryPlus.
45
By doing so, they earn rewards
as a credit to a designated spending or savings
account oered by the State Group health
plan or as a reimbursement for out-of-pocket
medicalexpenses.
In Nebraska, insurance carriers are required to
oer a program that gives 50% of the shared cost
savings to the enrollee, in cash or credit, when
the savings are $50 or more.
46
In Tennessee, they
also require insurance carriers to oer shared
savings incentives through cash, credit towards
the enrollees’ deductible, or reduction of a
premium, copayment, or cost sharing.
47
This can
be used in any state with price transparency laws
regardless of how comprehensive they may be.
Medicaid also oers a shared savings program
which has delivered savings for five years in
a row, including $1.6 billion in 2021, while still
providing high-quality care to patients.
48
Photo by CDC

14
Empowering Patients
Policy Proposals
Photo by Connor Betts
14
Empowering Patients

Empowering Patients
15
The federal rules under the Trump administration,
despite their good intentions, have not been
very successful to date because of the minimal
punishments and lack of enforcement. However,
they do lay a good foundation for the states
to implement their own price transparency
legislation. By codifying the federal rules, price
transparency will be protected in case the federal
rules are ever removed. Then states can also
adjust the legislation to make sure that it fits the
needs of their citizens, have better compliance,
and ultimately produce the healthcare savings
that price transparency makes room for. These
policies are likely to be popular with voters as
well, with recent polling showing that 87% of
Americans support rules that require hospitals to
disclose prices.
49
Model legislation
50
has been proposed that can
serve other states in implementing transparency.
This legislation mandates that each licensed
hospital in the state maintain a list that includes
payor specific charge information for a list
of “shoppable” procedures. If hospitals are
determined to be out of compliance with the
requirement, the legislation provides for fines
from the state. For example, in Colorado they do
not allow hospitals to go to collections on unpaid
bills if they are not in compliance, and in Texas,
top penalties could be $365,000 a year.
51
The next step would be to address surprise
billing. This may include building upon the federal
No Surprises Act by codifying and enforcing
the requirement for an Advanced Explanation
of Benefits (AEOB). When a patient schedules a
healthcare service at least ten days in advance,
the hospital and insurance company must
send them a good faith estimate within three
business days of what it will cost them.
52
It
includes information such as the amount the
insurance plan is paying and contracted rates of
in-network providers. This proposal would not
only make pricing information easier to access
for consumers, but also give more details to help
customers understand the context around pricing
and how they can compare their options. States
have codified and enforced the No Surprises Act
to varying degrees,
53
and ensuring the AEOB
could be a great next step. Other suggestions
for accessibility include requiring all healthcare
facilities, not just hospitals, to disclose prices,
have stricter penalties, and give state agencies
the necessary tools to enforce compliance.
Finally, states could provide incentives for
consumers to use the price transparency
tools available to them. As mentioned above,
states have done this by using shared savings
healthcare programs to reward state employees
for choosing lower-priced procedures, and
asking individual and small business markets
to do the same. These rewards can come in
the form of gift cards, lower premiums and
deductibles, or adding money to health savings
accounts. One way to test this out might be with
a pilot program as exemplified by Kentucky and
New Hampshire.
54
Policymakers interested in
this means of implementation should look to the
example of Florida discussed in the previous
section.
Other actions include ending out-of-network
discrimination so that patients understand other
options, giving smaller companies the ability to
see how their health care dollars are spent, and
banning anti-competitive contracting provisions.

16
Empowering Patients
Conclusion
While some like to use the cost of healthcare
as evidence of free-market failure, in reality the
healthcare marketplace hasn’t been “free” for
decades. From the creation of Medicare to the
Aordable Care Act to the expansion of Health
Maintenance Organizations under President
Nixon, the story of American healthcare is
one of an inexorable march toward putting
barriers between consumers and their care.
Price transparency is far from a silver bullet
for the rising cost of care, but would represent
a meaningful step toward giving power
back to consumers when it comes to their
healthcaredecisions.
Photo by Tima Miroshnichenko
16
Empowering Patients

Empowering Patients
17
1 https://www.statista.com/statistics/184968/us-health-expenditure-
as-percent-of-gdp-since-1960/
2 https://www.nbcnews.com/health/health-news/1-5-households-
medical-debt-includes-people-private-insurance-rcna48076
3 https://www.k.org/report-section/k-health-care-debt-survey-
main-findings/
4 https://www.k.org/health-reform/poll-finding/kaiser-health-
tracking-poll-late-summer-2018-the-election-pre-existing-
conditions-and-surprises-on-medical-bills
5 https://news.gallup.com/poll/269138/americans-delaying-medical-
treatment-due-cost.aspx
6 https://www.wmc.org/op-eds/reforms-needed-to-bring-down-
wisconsins-4th-highest-hospital-prices-in-the-country/
7 https://turquoise.health/service_oerings?q=CT+scan%2C+
head+or+brain%2C+without+contrast&service_name=ct-scan-
head-or-brain-without-contrast&location=53233&provider_
name=&sort=cost&page=1&distance=50
8 https://www.ncbi.nlm.nih.gov/pmc/articles/
PMC4863949#:~:text=These%20studies%20documented%20
large%20variations,outcomes%20(5%E2%80%938)
9 Out-of-Network Doctors at In-Network Hospitals - Consumer
Medical Bill Solutions (mymedicalbillsolution.com)
10 https://www.norc.org/NewsEventsPublications/PressReleases/
Pages/new-survey-reveals-57-percent-of-americans-have-been-
surprised-by-a-medical-bill.aspx
11 https://www.fiercehealthcare.com/hospitals/hospital-prices-widely-
vary-by-payer-often-higher-than-cash-price
12 https://www.thecentersquare.com/national/audit-of-hospital-
bailout-money-highlights-need-for-reform-health-oicials-say/
article_e8d563c2-9530-11ea-af5f-7756ed4accdc.html
13 https://www.k.org/report-section/ehbs-2021-
section-8-high-deductible-health-plans-with-savings-
option/#:~:text=Enrollment%20in%20HDHP%2FSOs%20
has,HSA%2Dqualified%20HDHPs%20in%202021
14 https://www.ehealthinsurance.com/resources/individual-
and-family/how-much-does-individual-health-insurance-
cost#:~:text=A%20deductible%20is%20the%20amount,and%20
%248%2C439%20for%20family%20coverage
15 https://www.healthcaredive.com/news/only-14-of-hospitals-comply-
with-federal-price-transparency-rules-advocac/618706/
16 https://www.aeaweb.org/articles?id=10.1257/pol.20150124
17 https://www.healthaairs.org/doi/full/10.1377/hltha.2015.0746
18 https://www.healthaairs.org/doi/10.1377/hltha.2015.0746
19 https://www.fiercehealthcare.com/hospitals-health-systems/report-
finds-barriers-to-use-price-transparency-tools
20 https://will-law.org/wp-content/uploads/2021/01/2019-08-09-
health_transparency_brief_final-ii.pdf
21 http://www-personal.umich.edu/~zachb/zbrown_eqm_eects_
price_transparency.pdf
22 https://www.cms.gov/hospital-price-transparency
23 https://www.cms.gov/files/document/steps-making-public-
standard-charges-shoppable-services.pdf
24 https://turquoise.health/
25 https://dashboard.sagetransparency.com/
Endnotes
26 https://www.cms.gov/healthplan-price-transparency
27 https://www.cms.gov/newsroom/press-releases/cms-oppsasc-
final-rule-increases-price-transparency-patient-safety-and-access-
quality-care
28 https://www.patientrightsadvocate.org/august-semi-annual-
compliance-report-2022
29 https://finance.yahoo.com/news/fga-files-lawsuit-against-
centers-202500390.html?guccounter=1
30 https://www.dol.gov/agencies/ebsa/laws-and-regulations/laws/no-
surprises-act
31 https://malegislature.gov/Bills/191/S2984
32 https://www.akleg.gov/basis/statutes.asp#18.23.400
33 https://www.mnhospitals.org/Portals/0/Documents/Member%20
Resources/MN_price_transparency_laws%286%29.pdf
34 https://www.tdi.texas.gov/health/healthprices.html
35 https://law.justia.com/codes/florida/2019/title-xxix/chapter-395/
part-i/section-395-301/
36 https://www.tn.gov/content/dam/tn/tacir/2020publications/2020_
RightToShop.pdf
37 https://nebraskamft.org/2022/01/27/legislative-update-
january-2022/
38 https://pub.njleg.gov/bills/2018/A2500/2039_I1.HTM
39 https://leg.mt.gov/bills/mca/title_0500/chapter_0040/part_0050/
section_0120/0500-0040-0050-0120.html
40 https://www.ncbi.nlm.nih.gov/pmc/articles/
PMC2837489/#:~:text=In%20California%2C%20hospitals%20
must%20provide,receive%20from%20a%20government%20payer
41 https://law.justia.com/codes/california/2005/hsc/1339.50-1339.59.
html
42 https://www.wipricepoint.org/Home.aspx
43 https://www.mybenefits.myflorida.com/content/
download/152414/1014218/Shared_Savings_Program_
FAQ_08.29.2019.pdf
44 https://www.healthcarebluebook.com/ui/home?path=direct
45 https://florida.surgeryplus.com/Client/ClientAccount/
Login?returnUrl=%2F
46 https://nebraskalegislature.gov/laws/statutes.php?statute=44-
1407&print=true
47 https://wapp.capitol.tn.gov/apps/BillInfo/default.
aspx?BillNumber=SB0510&GA=111
48 https://southfloridahospitalnews.com/medicare-shared-savings-
program-saves-medicare-more-than-1-6-billion-in-2021-and-
continues-to-deliver-high-quality-care/
49 https://www.patientrightsadvocate.org/feb2022surveyresults
50 https://alec.org/model-policy/hospital-price-transparency-act/
51 https://www.bizjournals.com/houston/news/2022/03/22/houston-
hospitals-price-transparency-baker-report.html
52 https://www.alaiahealth.com/articles/understanding-the-
advanced-explanation-of-benefits-provisions-in-the-no-surprises-
act#:~:text=to%20implement%20it.-,What%20Is%20An%20
Advanced%20Explanation%20of%20Benefits%3F,service%20is%20
as%20yet%20unscheduled
53 https://www.commonwealthfund.org/publications/maps-and-
interactives/2022/feb/map-no-surprises-act#map
54 https://www.tn.gov/content/dam/tn/finance/fa-benefits/documents/
shared_savings_incentive_programs_report.pdf

