
Tools for Developing
Police-Hospital Transition
Protocols in Ontario
May 2019
A COMPLEMENTARY GUIDELINE TO SUPPORT THE IMPLEMENTATION OF
IMPROVING POLICE-HOSPITAL TRANSITIONS: A FRAMEWORK FOR ONTARIO

Acknowledgements
Legal Disclaimer
This toolkit was developed in partnership with:
• Ministry of Health and Long-Term Care
• Ministry of the Solicitor General
• Provincial Human Services and Justice Coordinating Committee
• Canadian Mental Health Association (Ontario)
The information in this document is intended for information purposes
only. It does not provide legal or medical advice. If you have a health
question, you should consult a physician or other qualified health care
provider. If you have a legal question, you should consult a lawyer.
The information in this document is provided “as is” without any
representations or warranties, express or implied. Her Majesty the Queen
in right of Ontario (HMQ) makes no representations or warranties in
relation to any information in this document. HMQ does not warrant that
the information in this document is complete, accurate or up-to-date.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
1
Police-Hospital Transition Task Force
We would like to express our gratitude to all of the members of the Police-Hospital
Transition Task Force for their advice and guidance in the development of these tools
and resources.
Katie Almond and Michael Dunn, Provincial Human Services and Justice Coordinating
Committee
Fuad Abdi, Ministry of the Solicitor General
Nina Acco Weston and Alexia Jaouich, Centre for Addiction and Mental Health
Kashfia Alam, Human Services and Justice Coordinating Committee Secretariat
Jeffrey Bagg, Ontario Hospital Association
Alison Bevington, Waterloo Regional Police Service
Amanda Baine, Ministry of Health and Long-Term Care
Lisa Beck, Thunder Bay Regional Health Sciences Centre
Dena Bonnet, Ministry of the Attorney General
Brian Callanan, Toronto Police Association
Uppala Chandrasekera, Canadian Mental Health Association, Ontario
Raymond Cheng, Ontario Peer Development Initiative
Vanessa Aspri, Ministry of the Solicitor General
Theresa Claxton-Wali, Ontario Association of Patient Councils
Marg Connor, Ministry of Health and Long-Term Care
Sean Court, Ministry of Health and Long-Term Care
Sandra Cunning, Centre for Addiction and Mental Health
Alison DeMuy and Rebecca Webb, Waterloo-Wellington Local Health Integration Network
Ryan Fritsch, Legal Aid Ontario
Francine Gravelle, Youth Services Bureau
Paul Greenwood, St. Michael's Hospital
Lori Hassall, Canadian Mental Health Association, Middlesex Branch
Jenna Hitchcox, Human Services and Justice Coordinating Committee Secretariat
Ashley Hogue, Central Local Health Integration Network
Doug Lewis, Ontario Provincial Police Association
Phil Lillie, Provincial Human Services and Justice Coordinating Committee
Robyn MacEachern, Ontario Provincial Police
Diana McDonnell, Lanark County Mental Health
Terry McGurk, St. Joseph's Health Care Hamilton
John Pare, London Police Services and Ontario Association of Chiefs of Police
Stephen Waldie, Ministry of the Solicitor General
Margo Warren, Ministry of Health and Long-Term Care
Jeremy Watts, Alex Lam and Bryan Laviolette, York Region, Paramedic and Seniors
Services Branch
Mike Worster, Hamilton Police Service
Jodi Younger, St. Joseph's Health Care Hamilton

Tools for Developing Police-Hospital
Transition Protocols in Ontario
2
Overview
The following tools and resources have been developed as a complementary guideline to
support the implementation of Improving Police-Hospital Transitions: A Framework
for Ontario.
These tools and resources were developed based on existing promising practices in
Ontario. Their use is not a mandatory requirement, rather they are designed to help
police, hospitals and others comply with legal requirements (e.g. as found in Ontario’s
mental health, human rights, policing and privacy legislation) and best practices. These
tools may be tailored to the specific needs of local communities (except for Tool 4:
interRAI Brief Mental Health Screener which is a trademarked product).
The use of the term “hospital” throughout these documents refers to public hospitals
under the Public Hospitals Act, and the term “Schedule 1 Psychiatric Facilities” refers to
psychiatric hospitals which provide inpatient services and are designated under the
Mental Health Act.
Tool 1: Stages of Transition for an Individual in Crisis (pp.3-14)
This diagram provides a general overview of an individual’s
pathway from the moment of the onset of a mental health or
addictions-related crisis, to police officers arriving on the scene for
support, to their arrival at the hospital, through to their release back
into the community
Tool 2: Police-Hospital Committee Terms of Reference (pp.15-19)
This is a recommended template that may be adapted as needed
Tool 3: Police-Hospital Transition Protocol (pp.20-30)
This is a recommended template that may be adapted as needed
Tool 4: interRAI Brief Mental Health Screener (pp.31-34)
This is a recommended tool to support police officers when
responding to a mental health or addictions-related crisis situation
Tool 5: Transfer of Custody Form (pp.35-36)
This is a recommended template that may be adapted as needed

Tools for Developing Police-Hospital
Transition Protocols in Ontario
3
Tool 1: Stages of Transition for an Individual in Crisis
This diagram provides a general overview of an individual’s pathway from the moment
of the onset of a mental health or addictions-related crisis, to police officers arriving on
the scene for support, to their arrival at the hospital, through to their release back into
the community. This tool represents a simplified map of the pathway of an individual
that has been apprehended under the Mental Health Act. Each person’s pathway is very
different, and some journeys will not be reflected here. This map is meant only as a
general overview.
The Stages of a Police-Hospital Transition map can be used for two purposes:
• To inform users of the health care system about the general pathway to care that
an individual may experience if they are apprehended under the Mental Health
Act (map can be printed as a single page hand out for use with the general public
with shortened descriptions of each step and strategies).
• To educate hospital staff, police officers and other community service providers
involved with Mental Health Act apprehensions about the typical stages of
transition for the individual experiencing a mental health or addictions-related
crisis.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
Artwork by Rose Zgodzinski
For more information please visit www.hsjcc.on.ca

1.
Individual Experiences Crisis: When an individual is experiencing a mental health
or addiction-related crisis, the person requires care and attention to address their physical
and mental health needs while ensuring that they and others are kept safe in a difficult and
often unfamiliar situation. A mental health or addictions-related crisis can include: a
serious, immediate mental health or addictions problem, a situational crisis, psychosis, risk
of self-harm or harm to others, emotional trauma, agitation or inability to sleep as a result,
severe depression or anxiety, symptoms of moderate withdrawal and needing support, or
suicidal thoughts.
There are many individuals that may be involved to provide support during a crisis
situation, such as an individual’s family and friends, crisis centres, dispatch staff, police
officers, paramedics and emergency medical services, hospital staff, emergency nurses
and doctors, community mental health and addictions organizations and peer support
workers. In many communities, there are crisis services available that may be called before
911. ConnexOntario hosts an online listing of a community’s mental health and addictions
resources and operates a free, 24-hour crisis response line for mental health and
addictions-related concerns. For more information, visit:
www.connexontario.ca
2.
Crisis Call is Placed: When someone is experiencing a mental health or addictions-
related cr
isis, additional help for the person may be required and the individual or their
family may not know where to go for help. In these cases, friends, family members, or the
individual themselves may call a crisis line to seek assistance, such as ConnexOntario
which operates a free, 24-hour crisis response line: 1-866-531-2600. If crisis lines are not
available within a community, then 911 may be called for help.
3.
Police Officer Arrives: When the police are called or they come into contact with
an individual experiencing a crisis, they have a large role in determining the best course
of action to help the individual and ensure public safety. If the police officer determines
that the individual requires care for mental health or additions-related concerns, they may
apprehend the individual under the Mental Health Act.
4.
Mental Health Act Apprehension: Under the Mental Health Act, police officers
have t
he responsibility to take individuals who may be at risk of harming themselves or
others to an appropriate place for examination by a physician, often to a hospital
emergency department. Upon making the apprehension, the police officer remains with
the individual until transfer of custody to the hospital occurs. At this point, police officers
can use a mental health and addictions screening form (such as the interRAI Brief
Mental Health Screener) to document their observations of the individual apprehended
under the Mental Health Act. The individual may also be subject to a safety search by a
police officer at this time.
5.
Individual Taken to Emergency Department: An officer that has made an
apprehension under the Mental Health Act is required to transport the individual to a
psychiatric or health care facility. Often, the best option for immediate care for the
individual is the hospital emergency department. When arriving at the hospital, as part of
the intake process, the individual in crisis may be subject to a safety search.
6.
Joint Analysis of Risk: After arriving at the hospital, the police officer(s) and
hospital staff should jointly conduct an analysis of the level of risk the individual poses to
themselves and others within the hospital. Depending on the outcome of this risk
assessment, the police officers will either remain in the hospital or leave the individual in
the care of the hospital. If the police officers are no longer required, the individual has the
option of remaining in the hospital for an assessment by a physician to determine their
mental health care needs, or the individual may leave.
7.
Physician Examination: After an examination, the physician makes a decision
about whether a Form 1 is required. If the individual is issued a Form 1, there is the
authority to take the individual in custody to a psychiatric facility forthwith and detain the
individual for up to 72 hours for psychiatric assessment. If a Form 1 is not issued, the
individual can either stay voluntarily at the hospital for additional care, or they can leave.
Following this assessment, the physician or a hospital staff person may ask the individual
if the outcomes of this assessment can be communicated back to the police officer(s)
that apprehended the individual under the Mental Health Act.
8.
Individual Admitted: An individual can be voluntarily or involuntarily admitted to a
psychiatric f
acility once they have been assessed by a physician. If a Form 1 is issued and
an involuntary admission is made, the hospital then has the authority to hold custody of
the individual for up to 72 hours. Persons assessed on a Form 1 have a right to know the
outcomes of their assessment and potential detention, and to know of their right to counsel.
9.
Individual Released: Leaving an acute care setting for individuals that have
experienced a mental health or addictions-r
elated crisis requires good quality discharge
planning for a successful transition back into the community. Recovery from a crisis is
experienced differently by everyone. For many, it is important that the proper community
supports are put in place and connections or referrals to community programs are
provided. To keep an individual well within their community, it is important for hospital staff
to identify unique needs of individuals when released from the hospital.
A.
Planning for a Crisis: Crisis Planning helps to ensure client-centred care and offers
a way for individuals to establish a plan of action in preparation for periods of illness. Crisis
plans provide time-tested strategies for de-escalating crisis situations, provides the tools
for reducing triggers, and outlines specific treatments and medications that have either
mitigated or aggravated such experiences in the past. Individuals maintain the ability to
control the care they receive when they may be unable to effectively communicate. For
more information about crisis planning, see the Provincial Human Services and Justice
Coordinating Committee Information Guide: Strategies for Implementing Effective Police-
Emergency Department Protocols in Ontario (pg. 13-15) available at www.hsjcc.on.ca
B.
Mobile Crisis Response Teams: Mobile crisis response services may involve
health care professionals responding to a crisis or may involve a joint response between
police services and health care organizations. The joint response teams typically include
a police officer working alongside a mental health professional. Where available, these
response teams may be dispatched to assist the individual in crisis and they generally
arrive on the scene after the area has been made secure. The mobile crisis response team
assesses the individual in crisis and refers them to the appropriate place in the community
for care, whether it is a hospital or a community-based mental health and addictions
service provider.
C.
Using Community Resources: If a mental health apprehension is not made, police
officers can connect individuals to community resources in their area. ConnexOntario can
connect individuals in crisis (youth and adults), family and friends, and professionals with
information on types of services/programs and estimated wait times for support within their
community. The crisis response lines are staffed by Information and Referral Specialists
that are trained in suicide intervention skills and most have worked within frontline mental
health and/or addictions services. They engage in supportive listening with callers to help
ensure that individuals requiring support are linked to the most appropriate services in their
community. For more information, visit: www.connexontario.ca
D.
Calling Ahead: When police officers are en route to the hospital, it is best that the
police officers or the Police Service Communication Centre (dispatch) call ahead to inform
the emergency department staff that a mental health apprehension has taken place and
police officers will be arriving at their facility with the individual. This information allows
emergency department staff some additional time to adequately prepare for the incoming
individual.
E.
Communication Upon Arrival: Establishing communication between the police
officers and hospital staff upon arrival in the emergency department, and having the
officers provide all relevant information to hospital staff, can expedite the process and can
assist hospital staff in providing the best possible care to the person in crisis. Furthermore,
establishing strong communication upon arrival can help determine the length of time that
police officers will be required to remain at the hospital.
F.
Having a Quiet Room: Having a quiet space for individuals experiencing a crisis
can reduce the stigma associated with mental health and/or addictions conditions. The
quiet space provides privacy for the individual and offers shelter from the watchful eyes of
others waiting in the emergency room. A quiet space can also provide safety and security
for the individual in crisis.
G.
Designating a Liaison: A designated crisis coordinator in the emergency
department can be an asset to hospital staff as well as police officers in terms of
establishing clear communication. The designated crisis coordinator can also provide
services and supports to the individual experiencing a mental health or addictions-related
crisis, including conducting an initial mental health assessment, providing counselling
services, and connecting the individual to appropriate mental health and addictions
resources in the community.
H.
Peer Support: Some hospitals have peer support workers available within their
facility that can play a key role in supporting an individual in crisis. Having peer support
available for individuals experiencing a mental health or addictions-related crisis can help
the individual, family or other support people have conversations with a person that is
familiar with their situation and can assist with planning for any potential future crisis
situations that may arise.
I.
Low/Medium/High Risk Decision: An individual experiencing a mental health or
addictions-related crisis can be low, medium or high risk in harming themselves or others,
or fleeing from the hospital. The police officers and hospital staff should engage in a
conversation to collaboratively determine the risk level of the individual in crisis.
J.
Developing a Protocol for Transport: Non-Schedule 1 Facilities with emergency
departments should develop a protocol for transporting individuals who require a
psychiatric assessment to Schedule 1 Psychiatric Facilities. It is best practice that the
physician completing the Form 1 also provide a clinical assessment of how the individual
can be safely transferred to the new facility. The determination of transfer method and
rationale should be recorded by the physician. If paramedic services are needed for the
transport of the individual between facilities, the Provincial Transfer Authorization Centre
will need to be consulted during the development of the protocol.
K.
Documenting Transfer Efforts to Schedule 1 Facility: The Mental Health Act states
that the transfer of an individual to a Schedule 1 Psychiatric Facility for an assessment
needs to be completed “forthwith” which is generally interpreted in case law as “as soon
as reasonably possible.” It is recommended that the hospital staff document the efforts
made to transfer to the individual to the new facility, the care provided while waiting for the
transfer, and the ongoing monitoring and assessment of the individual to ensure that the
criteria for an individual to require a psychiatric assessment under Form 1 are still present.
L.
Ensuring Individual Rights and Freedoms: The hospital and police officers
responding to a crisis should take necessary steps to ensure that the individual’s right and
freedoms are protected at all times.
M.
Discharge Planning: Support from family, the community, and having access to the
social determinants of health (for example: housing and food) are key to increasing
wellness and preventing individuals from coming into contact with police or experiencing
additional, unanticipated visits to the emergency department. It is recommended that
discharge planning for individuals that have been frequently apprehended under the
Mental Health Act be reviewed by hospital staff to identify any gaps or issues that need
to be addressed to better connect individuals to community services while respecting the
individual’s right to treatment, choice and privacy.
Addictions, Mental Health, and Problem Gambling Treatment Services
Available 24/7: 1-866-531-2600
www.connexontario.ca
To
learn
more
about
individual
rights
when
a
Form
1
has
been
issued,
please
see
the
Community
Legal
Education
Ontario
resource
Are
you
in
hospital
for
a
psychiatric
assessment?
available
at:
http://www.cleo.on.ca/sites/default/files/book_pdfs/form1.pdf
For
individuals
seeking
additional
information
on
their
rights
while
in
the
care
of
an
Ontario
hospital
for
a
mental
health
or
addictions-related
concern,
contact
the
Psychiatric
Patient
Advocate
Office
at
1-800-578-2343
To
learn
more
about
the
legal
authorities
of
hospitals
to
detain
individuals
that
may
be
at
risk
to
harming
themselves
or
others,
please
see
the
Ontario
Hospital
Association
Practical
Guide
to
Mental
Health
and
the
Law
in
Ontario
available
at
www.oha.com

Tools for Developing Police-Hospital
Transition Protocols in Ontario
4
Stages of Transition for an Individual in Crisis
The stages of transition for individuals that have experienced a mental health or
addictions-related crisis and have been apprehended under the Mental Health Act are
described below. The strategies listed below are based on promising practices that have
been implemented in communities across Ontario. Please note that the strategies are
intended to support the development and implementation of a successful police-hospital
emergency department transition protocol and should be considered as
recommendations only, and are not mandatory requirements. Some strategies require
resources which may not be available in all communities.
1) Individual experiences a mental health or addictions-related
crisis
When an individual is experiencing a mental health or addictions-related crisis, the
person requires care and attention to address their physical and mental health needs
while ensuring that the person and others are kept safe in a difficult and often
unfamiliar situation. A crisis may require the assistance of professionals to help reduce
risks and provide care for the individual and others, especially if the circumstance is new
or unmanageable for the individual and those around them.
A mental health or addictions-related crisis can include: a serious, immediate mental
health or addictions problem, a situational crisis, psychosis, risk of self-harm or harm to
others, emotional trauma, agitation or inability to sleep and, as a result, severe
depression or anxiety, symptoms of moderate withdrawal and needing support, or
suicidal thoughts.
There are many individuals that may be involved to provide support during a crisis
situation, such as an individual’s family and friends, crisis centre dispatch staff, police
officers, paramedics and emergency medical services, hospital staff, emergency nurses
and doctors, community mental health and addictions organizations and peer support
workers.
In many communities, there are crisis services available for individuals experiencing a
mental health or addictions-related crisis that may be called before 911. ConnexOntario
Addiction, Mental Health, and Problem Gambling Treatment Services:
1-866-531-2600 | Available 24-hours every day
ConnexOntario: www.connexontario.ca

Tools for Developing Police-Hospital
Transition Protocols in Ontario
5
hosts an online listing of a community’s mental health and addictions resources and
operates a free, 24-hour crisis response line for mental health and addictions concerns.
2) Crisis call is placed
When someone is experiencing a mental health or addictions-related crisis, additional
help for the person may be required and the individual or their family may not know
where to go for help. In these cases, friends, family members, or the individual
themselves may call a crisis line to seek assistance. If crisis lines are not available within
a community, a 911 emergency call may be placed.
The role of the Police Service Communication Centre (dispatch) is important in the
response to individuals in crisis when a 911 call is placed. Particularly in communities
where there may be mobile crisis response teams that can be dispatched to a location to
assist police officers in their response, these teams can potentially divert individuals
away from emergency departments and the justice system, and offer care where the
individual is located. Crisis bed programs in the community may also be available to
support individuals in crisis.
ConnexOntario hosts an online listing of a community’s mental health and addictions
resources and operates a free, 24-hour crisis response line for mental health and
addictions concerns.
STRATEGY A: Planning for a crisis
I
ndividuals and families can develop a plan to prepare for a crisis situation.
C
risis Planning helps to ensure client-centred care and offers a way for
i
ndividuals to establish a plan of action in preparation for periods of illness. Crisi
s
p
lans provide time-tested strategies for de-escalating crisis situations, provide
th
e tools for reducing triggers, and outline specific treatments and medications
th
at have either mitigated or aggravated such experiences in the past.
I
ndividuals maintain the ability to control the care they receive when they may
be unable to effectively communicate.
For more information about crisis planning, see the Provincial Human Services
a
nd Justice Coordinating Committee Information Guide: Strategies for
I
mplementing Effective Police-Emergency Department Protocols in Ontario
(pp.13-15). www.hsjcc.on.ca

Tools for Developing Police-Hospital
Transition Protocols in Ontario
6
3) Police officer(s) arrive to assist the individual in crisis
When the police are called or they come into contact with an individual experiencing a
mental health or addictions-related crisis, they have a large role in determining the best
course of action to help the individual and ensure public safety. In some cases, there
may be a criminal incident that has also occurred at the same time as the mental health
or addictions-related crisis. In those situations, there may be times when a police officer
has to decide whether it is appropriate to make a mental health apprehension or to lay a
criminal charge. In appropriate circumstances, police officers should be encouraged to
make all efforts to divert a person away from the criminal justice system. Police officers
should give primary consideration to whether the Mental Health Act can appropriately
address the factors of concern in any particular case.
Police officers can connect individuals to community resources at any point. For
instance, where a criminal charge is not laid and a mental health apprehension is not
made, a police officer may connect the individual to community resources in their area.
ConnexOntario hosts an online listing of a community’s mental health and addictions
resources and operates a free, 24-hour crisis response line for mental health and
addictions concerns.
STRATEGY B: Utilizing mobile crisis response teams or other community
mental health and addictions agencies for support, where available
Mobile crisis response services may involve health care professionals responding
t
o a crisis or may involve a joint response between police services and health
c
are organizations. The joint response teams typically include a police officer
w
orking alongside a mental health and addictions professional. Where
a
vailable, these response teams may be dispatched to assist the individual in
c
risis and they generally arrive on the scene after the area has been made
s
ecure. The mobile crisis response team assesses the individual in crisis and refers
th
em to the appropriate place in the community for care, whether it is a hospita
l
or a community-based mental health and addictions service provider.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
7
ConnexOntario can connect individuals in crisis (youth and adults), family and friends,
and professionals such as police officers with information on types of services/programs
and estimated wait times for support within their community. The crisis response lines
are staffed by Information and Referral Specialists that are trained in suicide
intervention skills, most have worked within frontline mental health and/or addictions
services, and engage in supportive listening with callers to help ensure that individuals
requiring support are linked to appropriate services in their community.
4) Apprehension under the Mental Health Act
Under the Mental Health Act, when the required circumstances are met, police officers
have the authority to take individuals who may be at risk of harming themselves or
others to an appropriate place for examination by a physician, often to a hospital
emergency department. Upon making the apprehension, the police officer remains with
the individual until transfer of custody to the hospital occurs.
At this time, police officers can use the interRAI Brief Mental Health Screener form to
document their observations of the person apprehended under the Mental Health Act.
See Tool 4: interRAI Brief Mental Health Screener for more information.
During this process, the individual may also be subject to a safety search by a police
officer.
STRATEGY C: Using community resources, where available
If a criminal charge is not laid and a mental health apprehension is not made,
then police officers can connect the individual to community resources in their
area. For more information about community resources contact
ConnexOntario, which hosts an online listing of a community’s mental health
and addictions resources and operates a free, 24-hour crisis response line for
mental health and addictions concerns: www.connexontario.ca

Tools for Developing Police-Hospital
Transition Protocols in Ontario
8
5) Individual taken to the hospital emergency department
When the police officer(s) arrive at the hospital emergency department with the
individual experiencing a mental health or addictions-related crisis, a number of service
dynamics can occur during this transition process resulting in issues that impact on
police services, hospital staff and the individual in crisis. At this point, as part of the
intake process of the hospital, the individual in crisis may be subject to a safety search.
Establishing a Police-Hospital Transition Protocol is recommended to support everyone
involved in the transition. See Tool 3: Police-Hospital Transition Protocol for a general
template that may be adapted as needed.
STRATEGY D: Calling ahead
When police officers are en route to the hospital, it is best that the police officer(s)
or the Police Service Communication Centre (dispatch) call ahead to inform the
emergency department staff that a mental health apprehension has taken place
and the police officer(s) will be arriving at their facility with the individual. This
information allows emergency department staff some additional time to
adequately prepare for the incoming individual
STRATEGY E: Communicating upon arrival
Establishing communication between the police officer(s) and hospital staff upon
arrival in the emergency department, and having the officer(s) provide all
relevant information to hospital staff, can expedite the process and can assist
hospital staff to provide the most appropriate care to the individual in crisis.
Furthermore, establishing strong communication upon arrival can help determine
the length of time that police officers will be required to remain at the hospital.
Having a quiet space for individuals experiencing a crisis can reduce the stigma
associated with mental health and/or addictions conditions. The quiet space
provides privacy for the individual and offers shelter from the watchful eyes of
others waiting in the emergency room. A quiet space can also provide safety and
security for the individual in crisis.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
9
6) Joint analysis of risk
After arriving at the hospital, the police officer(s) and hospital staff should jointly
conduct an analysis of the level of risk the individual poses. The joint analysis of risk
should be completed by a designated hospital staff person (not necessarily a physician)
and the police officer.
The purpose of the joint analysis of risk is to determine whether the individual poses a
risk in harming themselves or others at the hospital, and whether the individual poses
a risk of fleeing from the hospital. In view of these particular risks, the designated
hospital staff person and the police officer should determine whether the hospital is
ready to take immediate custody of the individual such that the police officer(s) may
leave the hospital premises.
This risk analysis is distinct from the assessment associated with the decision about
whether to issue a Form 1. When required, the decision regarding issuing a Form 1
under the Mental Health Act rests solely with a physician.
STRATEGY G: Designating a liaison
A designated crisis coordinator in the emergency department can be an asset to
hospital staff as well as police officers in terms of establishing clear
communication. The designated crisis coordinator can also provide services and
supports to the individual experiencing a mental health or addictions-related
crisis, including conducting an initial mental health and addictions assessment,
providing counselling services, and connecting the individual to appropriate
mental health
and addict
ions resources in the community.
STRATEGY H: Peer support
Some hospitals within Ontario have peer support workers available within their
facility that can play a key role in supporting an individual in crisis. Having peer
support available for individuals experiencing a mental health or addictions-
related crisis can help the individual, family or other caregivers have
conversations with peers that are familiar with their situation and can assist with
planning for any potential future crisis situations that may arise.
Tools for Developing Police-Hospital
Transition Protocols in Ontario
10
At this point, a transfer of custody form can be used by hospital staff to document
decisions pertaining to the joint analysis of risk conducted by the hospital staff and the
police officer. See Tool 5: Transfer of Custody Form for a general template that may be
adapted as needed.
Strategy I: Low, Medium, High Risk Decision
An individual experiencing a mental health or addictions-related crisis can
be low, medium or high risk with respect to harming themselves or others, or
fleeing from the hospital. The criteria for high, medium and low risk should
be defined clearly and should appear on the transfer of custody form
keeping in mind the overarching goals of the protocol, specifically, to
improve and formalize the transition process.
If the individual is low-risk, the police officer(s) can transfer custody to the
hospital staff immediately.
Medium-risk individuals may or may not require the police officer(s) to stay.
To determine if the police officer(s) need to remain in the hospital, the
hospital staff and police officer(s) should engage in a conversation to
collaboratively determine the decision.
If the individual is high-risk, the police officer(s) must remain with the
individual until the individual has been assessed by a physician for the
purpose of determining whether to issue a Form 1.
An individual’s level of risk may fluctuate from low-to-high or high-to-low at
any time during or after the transition of custody. If the individual’s
observable behaviour indicates that they present a noticeable increased
risk of harm after the police officers have left, the hospital may call the
police to return – police services should prioritize these return calls.
It is best practice that if there is any dispute on the decision of the joint
analysis of risk, the police officer(s) should stay in the hospital at the request
of the hospital staff. If disagreement is persistent and systematic, police
services and the hospital may trigger their dispute resolution mechanism
through their Police-Hospital Transition Protocol to address the ongoing
issues.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
11
7) Physician’s Form 1 related examination
After an examination, the physician makes a decision about whether a Form 1 is
required (whether the test in Section 15 of the Mental Health Act is met). If the
individual is issued a Form 1, there is the authority to take the individual in custody to a
psychiatric facility forthwith and detain the individual for up to 72 hours for psychiatric
assessment. If a Form 1 is not issued, the individual can either stay voluntarily at the
hospital for additional care, or they can leave.
Following this assessment, the physician or a hospital staff person may ask the
individual if the outcomes of this assessment can be communicated back to the police
officer(s) that apprehended the individual under the Mental Health Act. The
individual’s consent to share or not to share information with the police officers should
be documented.
(7a) Transport to Schedule 1 Psychiatric Facility may be required
In some situations, the hospital where the person had been accompanied to by a police
officer does not have the legal authority to detain a patient on an involuntary basis.
Where this is the case, the person should be transported to a Schedule 1 Psychiatric
Facility
1
, that provides in-patient services, under the Mental Health Act for further
assessment and care.
A Form 1 is effective for seven days and provides authority to take the individual in
custody to a psychiatric facility where they may be detained, restrained, observed and
examined for no more than 72 hours.
1
A full list of designated Schedule 1 Psychiatric Facilities that provide in-patient psychiatric services in Ontario can be found here:
http://www.health.gov.on.ca/en/common/system/services/psych/designated.aspx
STRATEGY J: Developing a protocol for transport
Non-Schedule 1 Facilities with emergency departments should develop a protocol
for transporting individuals who require a psychiatric assessment at Schedule 1
Psychiatric Facilities. It is best practice that the physician completing the Form 1
may also provide a clinical assessment of how the individual can be safely
transferred to the new facility. The determination of transfer method and rationale
should be recorded by the physician. Should it be determined that paramedic
services are needed
for the transp
ort of the individual between facilities, the
Provincial Transfer Authorization Centre will need to be consulted when developing
the protocol as this is the body responsible for coordinating and approving all
transfers conducted by paramedic services in Ontario.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
12
Currently, within Ontario communities, the transport of the individual to a Schedule 1
Psychiatric Facility may be done by a family member, friend, paramedic services or
other patient transport service, or police officer(s). It is recommended that hospitals,
paramedic services, police services, and other appropriate transport entities ensure that
a process has been established for transporting clients to Schedule 1 Psychiatric
Facilities. This process can be embedded into the Police-Hospital Transition Protocol.
8) Individual is admitted to hospital
An individual can be voluntarily or involuntarily admitted to a Schedule 1 Psychiatric
Facility once they have been assessed by a physician. If a Form 1 is issued, the
hospital then has the authority to hold custody of the individual for up to 72 hours.
It should be considered best practice for hospitals to inform individuals assessed on a
Form 1 of their right to learn the reasons for their assessment and potential detention,
and be informed of their right to counsel, upon admission at the psychiatric facility.
Psychiatric facilities have certain obligations under the Mental Health Act, including
obligations to advise individuals of their rights (usually through delivery of a Form 42).
STRATEGY K: Documenting transfer efforts to Schedule 1 Psychiatric Facility
The Mental Health Act states that the transfer of an individual to a Schedule 1
Psychiatric Facility for an assessment needs to be completed “forthwith” which is
generally interpreted in case law as “as soon as reasonably possible.” It is
recommended that the hospital staff document the efforts made to transfer the
individual to the new facility, the care provided while waiting for the transfer, and
the ongoing monitoring and assessment of the individual to ensure that the
criteria f
or an individual to requ
ire a psychiatric assessment under Form 1 are still
present.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
13
STRATEGY L: Ensuring individual rights and freedoms
The following actions can be taken by hospital staff and police officers to
ensure that an individual’s rights and freedoms are protected in a crisis
situation:
As much as possible, it is recommended that hospital staff review internal
processes to ensure that individuals apprehended under the Mental
Health Act are quickly assessed, and that a decision for the hospital to
assume custody is made as early as possible (and so in compliance with
legislation). Hospitals can ensure that Canadian Triage Acuity Scale
(CTAS) levels being assigned to individuals presenting with mental health
or addictions-related crises are accurately reflecting acuity by internally
reviewing CTAS guidelines and how they are being applied within the
emergency department setting. Where all acuity is equal, the hospital
can put a process in place that prioritizes individuals accompanied by
police officers to be seen first in an effort to expedite the transition
process for individuals in crisis.
Provide supervised or monitored quiet rooms without locks.
Train hospital staff on the limits of their detention, search and restraint
powers, and alternative measures that may be used.
Train hospital and security staff on the legal rights framework, de-
escalation techniques, and human rights accommodations and privacy
requirements, with an emphasis on appropriate and effective
communication.
Train hospital staff on how to assess and triage apprehended persons
who are unable or unwilling to communicate.
Identify clear procedures around the provision of Form 42 and the
availability of peer support and advocacy services.
Additional resource for hospitals: To learn more about the legal authorities of hospitals
to detain individuals that may be at risk of harming themselves or others, please see the
Ontario Hospital Association Practical Guide to Mental Health and the Law in Ontario
available at www.oha.com

Tools for Developing Police-Hospital
Transition Protocols in Ontario
14
9) Individual is released from hospital
Leaving an acute care setting for individuals that have experienced a mental health or
addictions-related crisis requires good quality discharge planning for a successful
transition back into the community. Recovery from a crisis is experienced differently by
everyone. For many, it is important that the proper community supports are put in place
and connections or referrals to community programs are provided. To keep an
individual well once back in their community, it is important for hospital staff to work
with the individual to identify their unique needs when released from the hospital.
STRATEGY M: Discharge planning
The “revolving door” can occur in the emergency department. Police officers
m
ay accompany an individual apprehended under the Mental Health Act to
th
e emergency department; yet once the individual is examined by the
p
hysician, the individual may be released back into the community because
they did not meet the criteria for involuntary admission to a psychiatric facility.
Support from family, the community, and having access to the social
d
eterminants of health (for example: housing and food) are key to increasi
ng
w
ellness and preventing individuals from coming into contact with police or
experiencing additional, unanticipated visits to the emergency department.
It is recommended that discharge planning for individuals that have been
fr
equently apprehended under the Mental Health Act be reviewed by hospital
s
taff to identify any gaps or issues that need to be addressed to better connec
t
i
ndividuals to community services while respecting the individual’s right to
treatment, choice and privacy.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
15
Tool 2: Police-Hospital Committee Terms of Reference
This tool is a template for Ontario communities to use to assist with establishing a joint
police-hospital committee to support the development of a police-hospital transition
protocol. Communities can adapt and change this template to their local needs using
available resources. The purpose of this Terms of Reference document is to clearly
outline the role and scope of the Police-Hospital Committee, including the committee’s
objectives, membership, frequency of meetings and key contact information for matters
relating to police-hospital transitions and the corresponding protocol.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
16
Police-Hospital Committee Terms of Reference
(Insert date when Terms of Reference was created or revised)
Purpose of Police-Hospital Committee
The purpose of the committee is to bring together representatives from police services,
hospitals, paramedic services and community mental health and addictions
organizations in (insert name of your city/town) to develop and implement a police-
hospital transition protocol that complies with legal requirements and best practices
associated with Ontario’s mental health, human rights, policing and privacy legislation.
To support the work of this committee, members are encouraged to use Improving
Police-Hospital Transitions: A Framework for Ontario. The information, templates
and tools in this framework will provide guidance to members of this committee to
establish effective police-hospital transition protocols for individuals that have been
apprehended by police officers under the Mental Health Act and subsequently
accompanied to a hospital emergency department for assessment and care.
Objectives of Police-Hospital Committee
• To improve outcomes for people experiencing a mental health or addictions-related
crisis that are accompanied to an emergency department by a police officer while
respecting individual rights, including the right to privacy
• To enhance collaboration and coordination between hospitals and police services in
Ontario communities
• To decrease police officer wait times to transfer custody of apprehended individual to
hospital emergency department
• To protect health care worker safety and security through system improvements
• To promote public safety
• To identify strategies and solutions to any issues that may arise during the
implementation of the police-hospital transition protocol
• To develop strategies for ongoing monitoring and evaluation of the effectiveness of
the police-hospital transition protocol
• To annually review the work of this police-hospital committee and update the terms
of reference as necessary

Tools for Developing Police-Hospital
Transition Protocols in Ontario
17
Reporting Relationships
The (insert name of your committee) shall report to the Chief Executive Officer (CEO)
of (insert name of your hospital), and the Chief of Police of (insert name of your police
service) or Ontario Provincial Police (OPP) Detachment Commander. Paramedic
services and community mental health and addictions organizations are responsible for
reporting to their own respective organizations’ CEOs or their managers.
Responsibilities of Members
All members are responsible for attending Police-Hospital Committee meetings on a
regular basis and working to achieve committee objectives noted above. The
responsibilities outlined below indicate specific responsibilities of committee members.
Police Chief/OPP Detachment Commander and Hospital CEO will:
• Be the executive sponsors of the protocol
Police Designate with decision-making authority and Head of the Emergency
Department (i.e. the most senior person responsible for the Emergency Department,
such as a Chief of the Department, Vice President, Program Director, etc.) will:
• Provide guidance to staff on the successful implementation of the protocol and
resolve any disputes that may arise between the organizations
• Ensure all frontline staff complete the necessary training needed to implement
the police-hospital transition protocol
• Provide guidance to frontline staff throughout the implementation phase
• Ensure the ongoing monitoring and evaluation of the police-hospital transition
protocol
• Manage relationships and resolve issues between representatives of police
service(s), hospital and other members
Frontline police officers and hospital emergency department and privacy office staff
will:
• Deliver on the expectations associated with the written agreement between the
hospital and police service(s)
• Participate in all necessary training related to the police-hospital transition
protocol
• Work with other frontline police and hospital staff to implement the protocol
• Communicate progress and report any issues to their respective superiors

Tools for Developing Police-Hospital
Transition Protocols in Ontario
18
Other Service Provider Roles and Responsibilities:
• Deliver on the expectations associated with the protocol
• (Insert additional details)
Police-Hospital Committee Membership
Hospital representatives
Police representatives (can include multiple municipal police services and the OPP)
Paramedic Service representatives
Community Mental Health and Addictions Organization(s) representative(s)
Individual(s) with lived experience of police-hospital transitions
Police-Hospital Committee Meetings
Meetings will be held at least annually at (insert name of meeting location).
Meetings will be chaired by the Police Designate with decision-making authority and
Head of the Emergency Department (i.e. the most senior person responsible for the
Emergency Department, such as a Chief of the Department, Vice President, Program
Director, etc.).
Secretarial support for this Committee for minute-taking and other activities will be
provided by (insert name of organization).

Tools for Developing Police-Hospital
Transition Protocols in Ontario
19
Contact Information
For information about the Police-Hospital Committee, contact:
Hospital representative:
Title:
Telephone Number:
Email:
Police representative:
Title:
Telephone Number:
Email:

Tools for Developing Police-Hospital
Transition Protocols in Ontario
20
Tool 3: Police-Hospital Transition Protocol Template
This tool is a template for Ontario communities to use to assist with the development of
a police-hospital transition protocol. Communities can adapt and change this template
to their local needs using available resources. The purpose of this tool is to determine
the processes involved with police-hospital transitions when an individual has been
apprehended under the Mental Health Act.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
21
Police-Hospital Transition Protocol
(insert names/logos of partner organizations)
1. Introduction
This protocol is designed to enhance collaboration between hospitals and police
services with the purpose of improving outcomes for individuals that have been
apprehended by police officers under the Mental Health Act and subsequently
accompanied to a hospital emergency department for assessment and care.
The intent of this protocol is to 1) Improve outcomes for individuals apprehended by
police under the Mental Health Act, while respecting individual rights, including the
right to privacy; 2) Improve transitions between police officers and hospital workers;
and 3) Improve coordination and collaboration among partners involved in the
transition.
The protocol may be extended to include partnerships with other stakeholders in the
community, such as paramedic services, community-based mental health and
addictions agencies, peer and family support organizations, child and youth mental
health and addictions agencies and others.
2. Purpose
This protocol was developed in collaboration with key stakeholders who are the first
responders to individuals experiencing a mental health or addictions-related crisis.
This document reflects the commitment of all participants to provide an effective
and integrated response to such crisis situations in (insert name of your town/city).
The purpose of this agreement is to:
• To improve outcomes for people experiencing a mental health or addictions-
related crisis that are accompanied to an emergency department by a police
officer while respecting individual rights, including the right to privacy;
• To enhance collaboration and coordination between hospitals and police
services in Ontario communities;
• To decrease police officer wait times to transfer custody of apprehended
individual to hospital emergency department;
• To protect health care worker safety and security through system
improvements; and
• To promote public safety.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
22
This agreement outlines:
• The roles of the signatories in responding to the individual that has been
apprehended by police officers under the Mental Health Act; and
• The respective responsibilities of each signatory to ensure seamless transition
between frontline police officers and hospital staff.
3. Key Definitions
Mental Health: is the capacity of each and all of us to feel, think, and act in ways
that enhance our ability to enjoy life and deal with the challenges we face. It is a
positive sense of emotional and spiritual well-being that respects the importance
of culture, equity, social justice, interconnections and personal dignity.
2
Mental Illnesses: mental illnesses are health problems that affect the way we
think about ourselves, relate to others, and interact with the world around us.
They affect our thoughts, feelings, and behaviours. Mental illnesses can disrupt a
person’s life or create challenges, but with the right supports, a person can get
back on a path to recovery and wellness. It is important to understand that there
are many different types of mental illnesses that affect people in different ways.
3
Addiction: The term addiction is generally applied to patterns of heavy use of
psychoactive drugs that are taken primarily for their effects on consciousness,
mood and perception. In general, addiction has been replaced by the more
specifically defined term substance (or drug) dependence. However, “addiction”
continues to be used widely and is generally thought of as compulsive use leading
to physical symptoms of withdrawal when use is discontinued. For that reason, it
is often equated with physical dependence.
4
Form 1: This is the Application for Psychiatric Assessment and can be used to
bring someone to a psychiatric facility for an assessment that lasts up to 72 hours
(three days). To order a Form 1, a physician must have personally examined the
person within the previous seven days and have reason to believe that the person
meets certain criteria under the Mental Health Act. During the assessment, other
mental health professionals (e.g., nurses, psychologists and social workers) may
meet with the person and their family members, friends or caregivers to get
additional information.
5
2
Public Health Agency of Canada’s definition of mental health, taken from: http://www.phac-aspc.gc.ca/mh-sm/mhp-psm/index-eng.php
3
Canadian Mental Health Association’s definition of a mental illness, taken from: https://www.cmha.ca/mental_health/mental-illness/
4
Canadian Centre for Substance Abuse’s definition of addiction, taken from: http://www.ccsa.ca/Resource%20Library/ccsa-011811-2010.pdf
5
Centre for Addiction and Mental Health’s definition of Form 1, taken from:
http://www.camh.ca/en/hospital/visiting_camh/rights_and_policies/Pages/challenges_choices_appclegalform.aspx
Tools for Developing Police-Hospital
Transition Protocols in Ontario
23
Hospital and Schedule 1 Psychiatric Facility: Hospital refers to public
hospitals under the Public Hospitals Act, and Schedule 1 Psychiatric Facility
refers to psychiatric hospitals which provide inpatient services and are
designated under the Mental Health Act. Schedule 1 Psychiatric Facilities have
the legal authority to detain involuntary patients under the Mental Health Act,
and they provide inpatient mental health programs, including acute and short-
term care and treatment, to individuals experiencing mental health and
addictions related issues.
6
4. This protocol is between:
(List all organizations involved with the protocol)
Hospital
Police Service (can include multiple municipal police services and the OPP)
Paramedic Services
Community Mental Health and Addictions Organization(s)
(List any other partners)
5. Team Response
As soon as a Mental Health Act apprehension has been made and the police
officer(s) take the individual experiencing a mental health or addictions-related
crisis to the hospital emergency department, the following procedure will be
followed:
5.1) The police officer(s)/Police Service Communications Centre will advise the
hospital emergency department of the estimated time of arrival and that
an individual experiencing a mental health or addictions-related crisis will
be brought in for assessment.
6
A full list of designated Schedule 1 Psychiatric Facilities that provide in-patient psychiatric services in Ontario can be found here:
http://www.health.gov.on.ca/en/common/system/services/psych/designated.aspx

Tools for Developing Police-Hospital
Transition Protocols in Ontario
24
5.2) The police officer(s)/Police Service Communications Centre will share the
following information with the emergency department:
• Estimated time of arrival; and
• Whether the individual is being transported in a police vehicle or by
ambulance.
5.3) The responding police officer(s) will complete the interRAI Brief Mental
Health Screener (see Appendix for sample form). A copy of the completed
Form may be provided to (insert appropriate emergency department
staff position).
5.4) If the individual experiencing a mental health or addictions-related crisis
is being transported by police and their state as observed is such that
routine triage may not be appropriate or safe, the transporting officer(s)
will use the ambulance entrance of the hospital emergency department.
5.5) When an individual experiencing a mental health or addictions-related
crisis is brought to the hospital emergency department pursuant to the
Mental Health Act, the triage assessment will be completed by (insert
appropriate emergency department staff position).
6. Joint Analysis of Risk
After arriving at the hospital, the police officer(s) and hospital staff should jointly
conduct an analysis of the level of risk the individual poses. The joint analysis of
risk should be completed by a designated hospital staff person (not necessarily a
physician) and the police officer.
The purpose of the joint analysis of risk is to determine whether the individual
poses a risk in harming themselves or others at the hospital, and whether the
individual poses a risk of fleeing from the hospital. In view of these particular
risks, the designated hospital staff person and the police officer should determine
whether the hospital is ready to take immediate custody of the individual such
that the police officer(s) may leave the hospital premises.
This risk analysis is distinct from the assessment associated with the decision as
to whether to issue a Form 1. When required, the decision regarding issuing a
Form 1 under the Mental Health Act rests solely with a physician. Following the
assessment to determine if a Form 1 will be issued, the physician may ask the
individual if the outcomes of this assessment can be communicated back to the
police officer(s) that apprehended the individual under the Mental Health Act.
The individual’s consent to share or not to share information with the police
officers should be documented.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
25
The police officer shall remain with the individual until the transfer of custody
responsibility is complete. The transfer of custody is considered complete when
the responsible hospital staff member and police officer have reviewed the
Transfer of Custody Form and both have signed off in the designated areas (see
Appendix for sample form).
(In the following section, the criteria for high risk, medium risk and low risk
should be defined clearly and should appear on the transfer of custody form
keeping in mind the overarching goals of the protocol, specifically, to improve
and formalize the transition process.)
An individual experiencing a mental health or addictions-related crisis can be
low, medium or high risk:
• If the individual is low-risk, the police officer(s) can transfer custody to
the hospital staff immediately (add additional information as
appropriate).
• Medium-risk individuals may or may not require the police officer(s) to
stay. To determine if the police officer(s) need to remain in the hospital,
the hospital staff person and police officer(s) should engage in a
conversation to collaboratively determine the decision (add additional
information as appropriate).
• If the individual is high-risk, the police officer(s) must remain with the
individual until the individual has been assessed by a physician for the
purpose of determining whether to issue a Form 1 (add additional
information as appropriate).
An individual’s level of risk may fluctuate from low-to-high or high-to-low at any
time during or after the transition of custody. If the individual’s observable
behaviour indicates that they present a noticeable increased risk of harm after the
police officers have left, the hospital may call the police to return – police services
should prioritize these return calls.
It is best practice that if there is any dispute on the decision of the joint analysis
of risk, the police officer(s) should stay in the hospital at the request of the
hospital staff. If disagreement is persistent and systematic, police services and
the hospital may trigger their dispute resolution mechanism through their Police-
Hospital Transition Protocol to address the ongoing issues.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
26
7. Dispute Resolution
In the event of a dispute between the hospital and the police service concerning
any matter arising under this protocol, the Police Designate with decision-
making authority and the Head of the Emergency Department (i.e. the most
senior person responsible for the Emergency Department, such as a Chief of the
Department, Vice President, Program Director, etc.), shall meet, by telephone, or
in person, to engage in conversation to resolve the dispute.
In the event that any matter referred to the representatives set out above remains
unresolved after a period of 20 business days from its referral, then resolution
will fall to the Police Chief/OPP Detachment Commander and the Hospital CEO.
8. Forms to Complete
• interRAI Brief Mental Health Screener for use by frontline police officers to
document observations regarding the individual apprehended under the
Mental Health Act (see Appendix for sample form).
• A Transfer of Custody Form for use by hospital staff to document decisions
pertaining to a joint analysis of risk conducted by the hospital staff and the
police officer. The joint analysis of risk can be completed by a designated
hospital staff person (not necessarily a physician) and the police officer.
However, when required, the decision regarding issuing a Form 1 under the
Mental Health Act rests solely with a physician (see Appendix for sample
form).
9. Depending on the needs and resources available in your community,
insert the following:
Connecting Individual to Supports in the Community
(If community based agencies are involved with the police-hospital transition
protocol, then include the instructions for connecting the individual to supports
in the community here, including those related to respect for the individual’s
right to treatment, choice and privacy).
10. Information sharing associated with a Mental Health Act apprehension
Information sharing between police and hospital personnel concerning an
individual apprehended under the Mental Health Act will typically involve both
the individual’s personal information and their personal health information.
For example, a police officer’s observations about the individual will be the
individual’s personal information. When the hospital collects and uses
information for the purpose of providing health care to the individual, the
information is the individual’s personal health information.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
27
In sharing information, police, hospital and other emergency service partners
must be cognizant of their privacy-related obligations under relevant statutes
such as the Freedom of Information and Protection of Privacy Act, Health Care
Consent Act, Mental Health Act, Municipal Freedom of Information and
Protection of Privacy Act and Personal Health Information and Protection Act.
This means that the disclosing organization must have the authority to disclose
and the recipient organization must have the authority to collect and use the
personal information and/or personal health information at issue.
In this context, it is noteworthy that hospital staff must generally comply with the
limiting principles set out in Section 30 of the Personal Health Information and
Protection Act. Section 30 generally requires that no personal health information
be collected, used or disclosed if other information will serve the purpose and
that no more personal health information be collected, used or disclosed than is
reasonably necessary to meet the purpose. Similar limiting principles also apply
to the collection, use and disclosure of personal information by police under
Municipal Freedom of Information and Protection of Privacy Act.
10.1) Disclosures and collections related to apprehension and transport
Under the Mental Health Act, police officers have the authority to take
individuals who may be at risk of harming themselves or others to an appropriate
place for examination by a physician, often to a hospital emergency department.
In the course of apprehending an individual under Section 17 of the Mental
Health Act, police officers may collect relevant information about an individual’s
demeanor, behavior and circumstances, and use that information to safely
apprehend and transport that individual to hospital.
While in transit, police officers may call ahead to inform the emergency
department staff that a mental health apprehension has taken place and police
officers will be arriving at their facility with the individual. In addition, upon
arrival in the emergency department, police officers may disclose further
personal information to hospital staff where that information is reasonably likely
to be relevant to the hospital’s safe assessment, treatment, detention and release
of the individual, including information describing the officers’ observations
about the individual’s demeanor, behavior and circumstances.
As health information custodians, hospitals can only collect, use and disclose
personal health information in accordance with the rules set out in the Personal
Health Information Protection Act including the limiting principles set out in
section 30.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
28
Reasonable care should be taken by both police officers and hospital staff to
ensure that information sharing be restricted to information that is as accurate,
complete and up-to-date as possible.
10.2) Disclosures and collections related to transfer of custody
Upon making the apprehension, police remain with the individual until transfer
of custody to the hospital occurs. The Mental Health Act regulations require that:
a decision about the transfer of custody be made as soon as is reasonably
possible; the hospital decision maker consult with the police officer(s); and
hospital staff promptly inform the police of the decision.
Under this protocol, the transfer of custody generally occurs under one of the
following two circumstances:
1. Custody of an individual may pass from police to the hospital where the
responsible hospital staff member and police officer have reviewed the
Transfer of Custody Form; agreed that the hospital is ready to take immediate
custody of the individual; and signed the designated areas of the Transfer of
Custody Form.
In informing the police of this transfer decision, the hospital should restrict its
disclosure of personal health information to the police to the information on
the Transfer of Custody Form.
2. Where the responsible hospital staff member and police officer have
determined that the police officer should remain at the hospital until a
physician has decided whether to issue a Form 1, custody of an individual may
pass from police to the hospital after the physician has made the Form 1
decision.
Following an initial examination, hospital staff can inform the police officers
of their decision to issue or not issue a Form 1 for the individual if the police
officer has remained in the hospital. But if this assessment has occurred after
the police officers have passed custody to the hospital and left the hospital
premises, the hospital staff may ask the individual if they consent to sharing
this information (whether the individual is admitted or not).
If the police ask the hospital to disclose whether the individual is ultimately
detained under a Form 1, the hospital may inform the police officer as to
whether or not a Form 1 was issued with the express consent of the individual.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
29
As a general rule, the hospital should only ask the individual to consent to this
disclosure of their personal health information after the Form 1 decision has
been made. Moreover, in order to ensure that the consent is knowledgeable
and freely given, the individual must be informed of the specific personal
health information that will be disclosed to the police (i.e. that a Form 1 has
been issued or that no Form 1 has been issued), the specific purpose(s) for the
disclosure, and the individual has the right to give or withhold consent to the
hospital’s disclosure of this personal health information. In addition, the
individual should be informed that this disclosure of personal health
information could lead to further mental health-related disclosures by the
police (e.g. about the issuance of a Form 1 to other police services through the
Canadian Police Information Centre).
In addition, the individual must be capable of consenting to any disclosure of
their personal health information, which includes information regarding the
issuance of a Form 1. The test for consent to the collection, use and disclosure
of personal health information is set out in s. 21 of the Personal Health
Information Protection Act (PHIPA).
10.3) Other disclosures and collections
An individual’s level of risk may fluctuate during or after the transition of custody
phase. If an individual’s observable behavior indicates that they present a
noticeably increased risk of harm after the officers have left (e.g. to another
person or to themselves), the hospital may call the police and ask them to return
to the hospital or assist in the re-location of the individual.
Authority for such a disclosure is found in Section 40(1) of the Personal Health
Information and Protection Act which permits a hospital to disclose personal
health information if the hospital believes on reasonable grounds that the
disclosure is necessary for the purpose of eliminating or reducing a significant
risk of serious bodily harm to a person or group of persons. “Significant risk of
serious bodily harm” includes a significant risk of both serious physical as well as
serious psychological harm. Like all collection, use and disclosure provisions of
the Personal Health Information and Protection Act, Section 40(1) is subject to
the limiting principles in Section 30.
It is understood and agreed that the parties in this protocol shall hold all
information, materials and client information gained through participation in
this agreement in confidence in accordance with each organization’s policies.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
30
11. Joint Training
Training will be an important component of our ability to better serve the
individual experiencing a mental health or addictions-related crisis. Our partners
are committed to assisting each other in their training needs. Training will be
constantly modified to enhance our ability to serve the individual experiencing a
mental health of addictions-related crisis.
(Insert training details)
12. Contact Information
For more information about this protocol, contact:
Hospital representative:
Title:
Telephone Number:
Email:
Police representative:
Title:
Telephone Number:
Email:
13. Signatories
(Signatures from all organizations involved with the protocol)
Hospital
Police Service (can include multiple municipal police services and the OPP)
Paramedic Services
Community Mental Health and Addictions Organization(s)
(List other partners here)

Tools for Developing Police-Hospital
Transition Protocols in Ontario
31
Tool 4: interRAI Brief Mental Health Screener
The interRAI Brief Mental Health Screener provides police officers with a tool to assist
in identifying persons experiencing a mental health or addictions-related crisis. This
tool enables police officers to record their observations about the individual in crisis and
articulate their observations to appropriate health care professionals. The use of the
interRAI Brief Mental Health Screener is recommended for police services across
Ontario.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
32
About the interRAI Brief Mental Health Screener
The interRAI Brief Mental Health Screener (BMHS) provides police officers with a tool
to assist in identifying persons experiencing a mental health or addictions-related crisis.
It enables police officers to record their observations about the individual in crisis and
articulate their observations to appropriate health care professionals. The purpose of
BMHS is to develop an effective way of documenting the observations made by the
police officers at the time of the crisis/incident so as to better inform and support
decision-making by staff in the emergency department. The ultimate goal underlying the
development and use of the BMHS is to ensure that people experiencing a mental health
or addictions-related crisis who come into contact with police officers receive prompt
access to appropriate health care services, reducing the risk of criminalization.
Core items on the BMHS were extracted from a sample of 40,000 cases in the Ontario
Mental Health Reporting System database for the Resident Assessment Instrument for
Mental Health (RAI-MH) version 2.0, which is the psychiatric assessment tool used with
all patients admitted to psychiatric hospital beds in the province of Ontario. Additional
items were identified through collaboration with police officers, hospital staff, and
mental health and addictions professionals. A pilot study was conducted over an eight-
month period with the participation of two police services, four general hospitals and
one psychiatric facility in southern Ontario. The effectiveness of the BMHS was
demonstrated by testing the association between police officers’ ratings on the form and
clinicians’ assessments conducted in the emergency department of the general hospitals.
There are two major benefits to using the BMHS. First, when police officers learn to use
the BMHS, they are receiving enhanced evidence-informed training on the key
indicators of mental health and addictions conditions. Second, because the core items
on the BMHS mirror that of the RAI-MH tool, police officers are using a form that is not
only based on health system data but also written in health system language. Using
common language acts as a bridge between the two sectors, thus laying the foundation
for a more collaborative approach between hospitals, police services and community
mental health and addictions service providers.
The BMHS does not replace a police officer’s authority under the Mental Health Act.
Police officers complete the BMHS for all persons presenting with a mental health or
addictions-related crisis regardless of the officer’s intended course of action (i.e. release,
referral, diversion, Mental Health Act apprehension, arrest for criminal offence, etc.). A
copy of the BMHS is provided to emergency department staff or to community mental
health and addictions service providers, as the BMHS may be used by emergency
department staff to assist in their assessment, and community mental health and
addictions service providers may use the form to determine whether follow-up care is
necessary with the individual.

Tools for Developing Police-Hospital
Transition Protocols in Ontario
33
interRAI Brief Mental Health Screener Demonstration Copy
Copies of this form are available at minimal cost. For more information, visit:
https://catalog.interrai.org/category/bmhs-forms
Tools for Developing Police-Hospital
Transition Protocols in Ontario
34
Accessing the interRAI BMHS
To use the BMHS, a police service must sign a User Agreement with interRAI and agree
to purchase BMHS manuals for training purposes (manuals are available online at a
minimal cost: https://catalog.interrai.org/category/bmhs-manuals). There are various
ways that police officers can convey the information on the BMHS to health care
professionals, from hand delivery to electronic transmission. To determine which
method is most appropriate for your police service and to obtain a copy of the BMHS
User Agreement please contact:
Dr. Ron Hoffman
School of Criminology and Criminal Justice
Nipissing University, 100 College Drive, Box 5002
North Bay, Ontario, P1B 8L7
Tel: (705) 474-3450 ext. 4565
Email: r[email protected]
Development of the interRAI BMHS
There were several stages to the development of the interRAI BMHS including a focused
literature review, an analysis of the RAI-MH database, the creation of a research team
and advisory committee.
7
Input was also solicited from interRAI researchers and in
particular the interRAI Network of Mental Health (iNMH) which was established in
2005 to support research and implementation of the interRAI mental health
instruments. The iNMH is comprised of about 30 researchers and clinicians from nine
countries (Canada, United States, Finland, Iceland, Netherlands, Australia, Brazil, Chile,
Peru, Russia) with a broad range of expertise in mental health services.
About interRAI
interRAI is an international collaborative network of researchers in over thirty
countries committed to improving the quality of life of vulnerable persons through a
seamless comprehensive assessment system. As a not-for-profit consortium, interRAI
strives to promote evidence-informed clinical practice and policy decision making
through the collection and interpretation of high-quality data about the characteristics
and outcomes of persons served across a variety of health and social services settings.
For more information about interRAI, visit: www.interrai.org
7
For more information about the interRAI BMHS, see: Hoffman, R. et al. (2016). The use of a brief mental health screener to enhance the ability of
police officers to identify persons with serious mental disorders. International Journal of Law and Psychiatry, 47, 28-35. Retrieved from
http://www.sciencedirect.com/science/article/pii/S0160252716300449

Tools for Developing Police-Hospital
Transition Protocols in Ontario
35
Tool 5: Transfer of Custody Form
This tool is a template for Ontario communities to use to assist with the development of
a police-hospital transition protocol. Communities can adapt and change this template
to their local needs using available resources.
This form is used to document the joint analysis of risk conducted by the police
officer(s) and hospital staff. The purpose of the joint analysis of risk is to determine
whether the individual poses a risk with respect to harming themselves or others, and
whether the individual poses a risk of fleeing from the hospital. The outcome of this
analysis is to determine if the police officer(s) can transfer custody of the individual to
the hospital staff or remain in the hospital. The joint analysis of risk should be
completed by a designated hospital staff person (not necessarily a physician) and the
police officer(s).
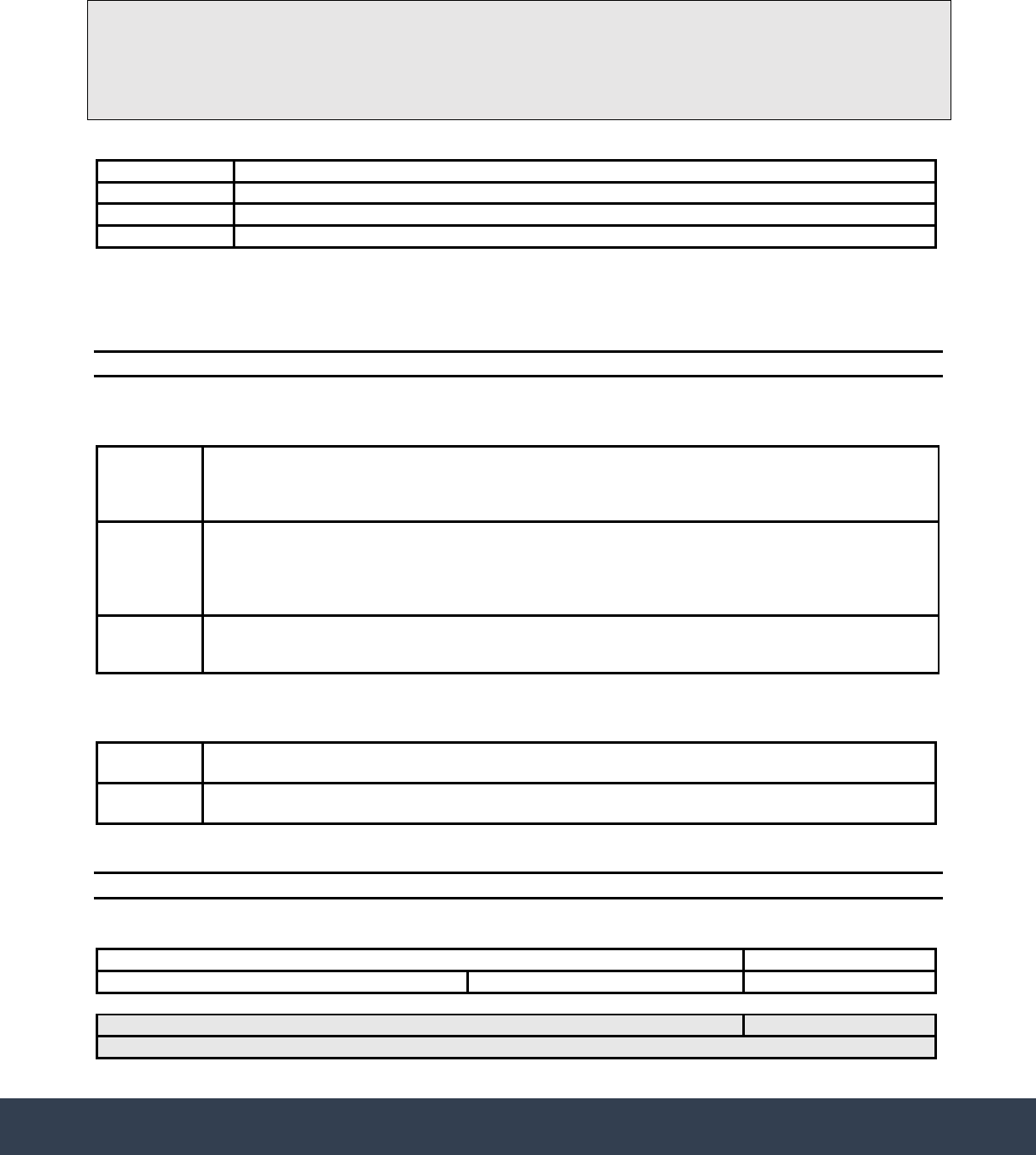
Tools for Developing Police-Hospital
Transition Protocols in Ontario
36
Transfer of Custody Form
Personal Information
Name
Address
Telephone
Date of Birth
interRAI Brief Mental Health Screener Completed by Officer(s):
No
Yes BMHS form attached
Behaviour(s) Observed:
Disposition
Disposition of the individual. Descriptors are guidelines only.
High Risk
Many verbal and physical indicators are demonstrated in the past 30-minutes. Individual is not
cooperative. Has a history of violence or of absconding from institutions. Recent substance abuse. If
the individual is high-risk, the police officer(s) must remain with the individual until the individual
has been assessed by a physician for the purpose of determining whether to issue a Form 1.
Mediu
m
Risk
Some verbal and physical indicators are demonstrated in the past 30-minutes. Individual is
cooperative some of the time. May have a history of violence or absconding from institutions. May
have had recent substance abuse. Medium-risk individuals may or may not require the police
officer(s) to stay. To determine if the police officer(s) need to remain in the hospital, the hospital staff
and police officer(s) should engage in a conversation to collaboratively determine the decision.
Low Risk
Individual is docile and cooperative during the past 30-minutes. No history of violence or absconding
from institutions. No recent substance abuse. If the individual is low-risk, the police officer(s) can
transfer custody to the hospital staff immediately.
Action
Did the Police Officer leave the individual at the hospital?
Yes
Time Officer left:
No
Officer remained for the following reasons:
Additional Comments or Observations:
The signatures below indicate agreement with the behaviour(s) observed and the disposition checked:
Hospital Staff:
Time:
Police Officer: Badge Number: Time:
Police Officer returned to the facility: Time:
Reason:
This
form
is
used
to
document
the
joint
analysis
of
risk
conducted
by
the
police
officer(s)
and
hospital
staff.
The
purpose
of
the
joint
analysis
of
risk
is
to
determine
whether
the
individual
poses
a
risk
with
respect
to
harming
themselves
or
others
at
the
hospital,
and
whether
the
individual
poses
a
risk
of
fleeing
from
the
hospital.
The
outcome
of
this
analysis
is
to
determine
if
the
police
officer(s)
can
transfer
custody
of
the
individual
to
the
hospital
staff
or
remain
in
the
hospital.
The
joint
analysis
of
risk
should
be
completed
by
a
designated
hospital
staff
person
(not
necessarily
a
physician)
and
the
police
officer(s).

Additional Resources
Hoffman, R. et al. (2016). The use of a brief mental health screener to enhance the ability of
police officers to identify persons with serious mental disorders. International Journal
of Law and Psychiatry, 47, 28-35.
http://www.sciencedirect.com/science/article/pii/S0160252716300449
Ontario Hospital Association. (2012). Practical Guide to Mental Health and Law in
Ontario.
http://www.oha.com/CURRENTISSUES/KEYINITIATIVES/MENTALHEALTH/Page
s/MentalHealthandtheLaw.aspx
Provincial Human Services and Justice Coordinating Committee. (2013). Strategies for
Implementing Effective Police-Emergency Department Protocols in Ontario.
http://www.hsjcc.on.ca/Provincial/Planning%20and%20Priorities/Strategies%20for%
20Implementing%20Effective%20Police-
Emergency%20Department%20Protocols%20in%20Ontario.pdf
Public Services Health & Safety Association. (2013). Completing the
Violence/Aggression Assessment Checklist (VAAC) for Emergency Departments (ED)
or Emergency Medical Services (EMS). https://www.pshsa.ca/wp-
content/uploads/2013/02/VAACEtoo_-instruction.pdf.pdf
Relevant Legislation can be accessed at: https://www.ontario.ca/laws
• Freedom of Information and Protection of Privacy Act, 1990
• Mental Health Act, 1990
• Municipal Freedom of Information and Protection of Privacy Act, 1990
• Personal Health Information Protection Act, 2004
37
Tools for Developing Police-Hospital
Transition Protocols in Ontario

